The Specialists in one Center of Excellence
Carpal tunnel syndrome is the most common peripheral nerve compression syndrome. According to international studies, approximately 15% of adults will be affected by this condition at some point in their lives. Despite conservative treatment options most cases require surgery, specifically carpal tunnel release. It is the most common surgical procedure and should be performed by an experienced hand surgeon. In Germany it is carried out more than 300,000 times, in 90% of the cases on an outpatient basis. According to recent scientific studies, up to 30% so-called amyloid deposits in the tendon gliding tissue or carpal ligament are found intraoperatively or in the pathological processing of the biopsy material taken in carpal tunnel syndrome patients over 50 years of age. These deposits can spread systemically through the body and lead to amyloid cardiomyopathy with the symptoms of heart failure. Therefore, a very careful surgical technique with the removal of tissue samples makes sense for the pathologist. If any amyloid deposits are discovered, a cardiological clarification is required immediately. Prof. Dr. Dr. Sauerbier has extraordinarily extensive experience in this operation and has carried out the procedure in the high four-digit range.
The Carpal Tunnel Syndrome Center of Excellence bundles diagnostics, physician’s therapy or hand-therapeutic treatment of the disease respectively, with the latest methods in neurological examination and imaging (high-resolution nerve ultrasound examination, MRI if required), followed by an interdisciplinary team assessment for the benefit of the patient.
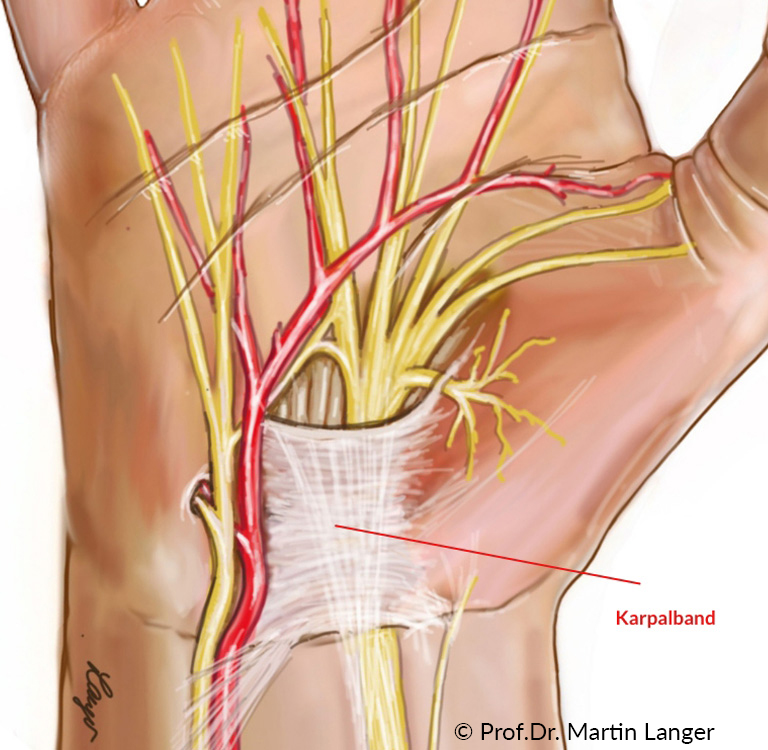
The symptoms of carpal tunnel syndrome (CTS) are due to pressure damage to the median nerve (middle nerve) in the so-called carpal tunnel (bony connective tissue canal in the carpal bones). There is a mismatch between the width and content of the carpal tunnel. The median nerve supplies the thumb, index, middle and ring fingers (thumb side) with and the thenar muscles with strength. The main symptoms of the disease are hands that go to sleep at night (so-called brachialgia paresthetica nocturna), often associated with pain in the hand or the entire arm. Tingling paresthesias or pinprick-like sensations are mainly found on the fingers supplied by the median nerve. The symptoms can also occur during certain activities at work, when riding a bicycle or motorbike, making phone calls, etc., and can be alleviated by shaking out the hand, changing the position of the hand or immobilizing it in a splint. In the advanced clinical scenario, there is a pronounced numbness of the affected fingers and fine gripping work can hardly be carried out. In the late stage, there is usually a reduction in the muscle mass of the ball of the thumb combined with weakness of the thumb in extension and opposition.
The age of onset is usually between 40 and 70 years of age, and in over 50% of cases there is a need for treatment on both sides. Women are significantly more likely to suffer from carpal tunnel syndrome than men. t is not uncommon for carpal tunnel syndrome to contain so-called amyloid deposits in the tissue around the median nerve, which can also lead to heart disease (amyloid cardiomyopathy or heart failure).
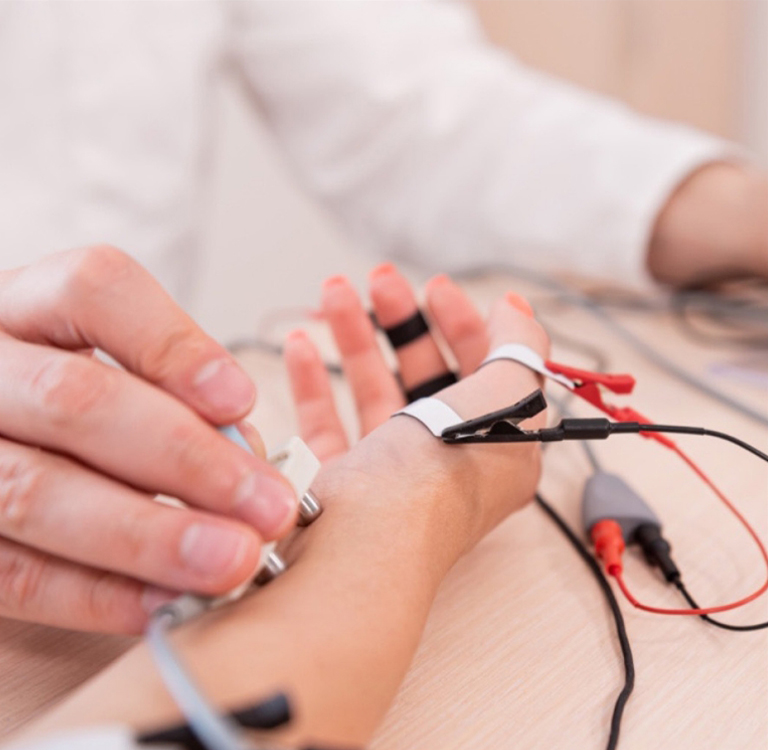
Carpal tunnel syndrome is a dysfunction of the nerve (median nerve) in the wrist area. The nerve fibers, however, can also be damaged along the arm or in the cervical spine. To determine the exact location of the damage, different examinations are mostly combined. Through motor and sensory electroneurography, the nerve conduction velocities can be measured in the wrist, forearm or upper arm. The nerve is stimulated by small current pulses and registers the stimulus response via surface electrodes. When examining the SSEP (somatosensitive evoked potentials) the nerve in the wrist is stimulated and the response to the stimulus is recorded via then scalp od the patient with two acupuncture needles. Thereby, in particular, proximal / near spine damage, due to herniated disc for example, can be detected. The electrophysiological study can secure the diagnosis of carpal tunnel syndrome, others rule out causes of damage and is suitable for monitoring the course of nerve function
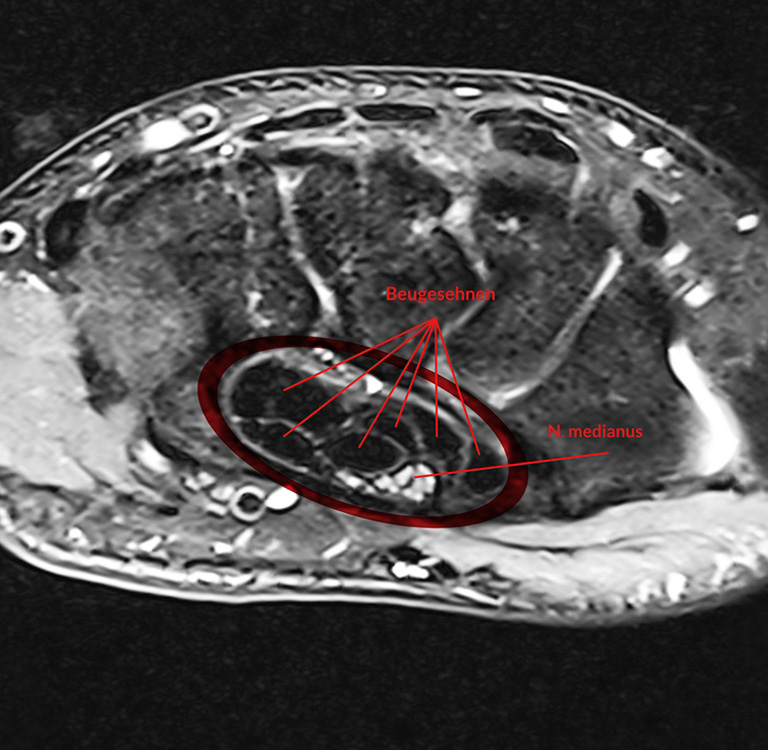
The diagnosis of carpal tunnel syndrome is based on anamnesis, physical examination and measurement of the nerve conduction velocity. In addition, a high-resolution magnetic resonance imaging specially designed for such cases can be used (MRI) on modern devices with high field strength to demonstrate a high percentage of typical changes in the median nerve, for example, a nerve compression within the carpal tunnel. Additional changes in the carpal canal – for example, through inflammatory processes or tumors – as the primary cause of carpal tunnel syndrome, can also be found with MRI. In contrast to computed tomography (CT), MRI does not require potentially harmful X-rays, so it can – usually for other cases – can also be used with children without any problems.
It occurs often that conservative measures such as splint treatment at night, hand therapy, manual therapy, and injection treatment with cortisone did not alleviate the symptoms. In these very common cases, only surgical therapy or carpal tunnel release leads to success.
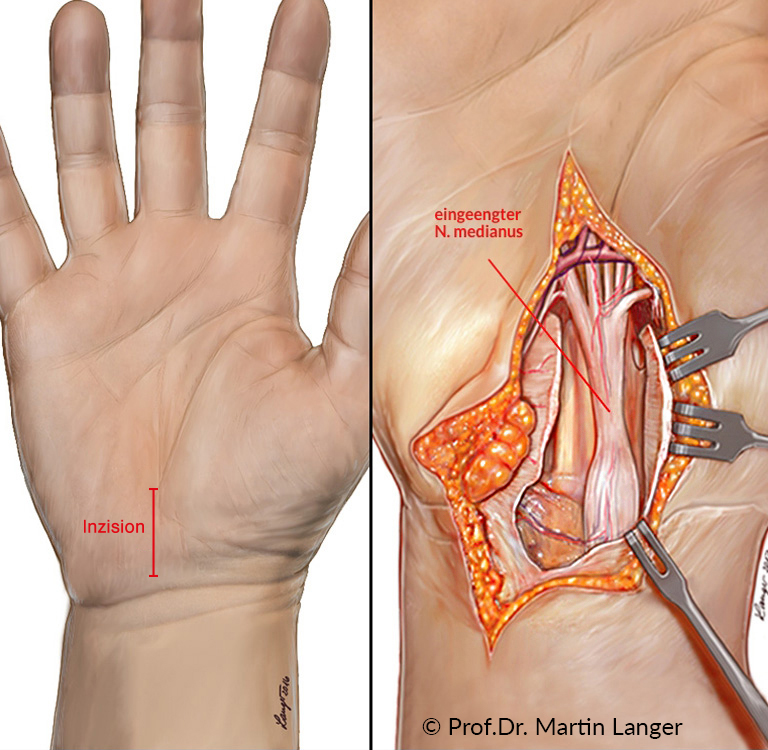
The open carpal tunnel release is the standard procedure and is performed far more frequently than the endoscopic technique. It is carried out either under local anesthesia (so-called Wide Awake procedure: WALANT) or brachial plexus anesthesia, in exceptional cases also under general anesthesia. The operation is performed under loupe magnification. The skin incision runs just above the carpal tunnel with a length of 3-4 cm. The carpal ligament (retinaculum flexorum) is completely severed with a scalpel. Optimal visualization is important.
For depiction of the median nerve (N. medianus). In the case of pronounced thickening of the flexor tendon gliding tissue in the carpal tunnel, a removal is necessary of the gliding tissue is required to get space for the nerve. In addition, a tissue sample should be taken so that a so-called transthyretin amyloidosis, which can lead to amyloid heart muscle disease, can be ruled out after examination by the pathologist. After the skin is sutured, a loose cotton bandage is applied and, if necessary, immobilization in a splint. The suture material is removed after 12-14 days. With independent movement exercises, the patient can start on the day of the operation after the anesthetic has worn off. Professional hand therapy is recommended from the 1st day after the operation.

Private Medical Practice for Hand and Plastic Surgery
Michael Sauerbier MD PhD
Specialist in Plastic, Reconstructive and Aesthetic Surgery – Hand Surgery
- Louisenstraße 92 • 61348 Bad Homburg v. d. Höhe






